From technical hurdles to ethical dilemmas, healthcare providers face numerous obstacles using AI in healthcare–in particular, how to implement AI in clinical practice. A 2023 survey by the American Medical Association found that 93% of doctors believe AI can improve patient care, but only 38% feel prepared to use it in their practice.
In this article, we’ll delve into the obstacles and potential solutions to implementing AI in healthcare and integrating AI into an existing health system.
Contents
- Challenges with Implementing AI in Healthcare
- How to Implement AI Platforms in Healthcare
- Conclusion
Challenges with Implementing AI in Healthcare

High integration costs
Implementing AI in healthcare is expensive. It takes a significant investment to buy the systems, manage data, and train staff:
- High Initial Investment for AI Implementation: The cost of acquiring and implementing AI systems can be prohibitive for many healthcare providers. These costs include computers, data storage, and patient data security.
- Ongoing Costs for Maintenance and Upgrades: AI systems require continuous maintenance and updates, adding to the overall cost.
- Balancing AI Spending with Other Healthcare Priorities: Healthcare providers must balance AI investments with other critical healthcare needs.
To make a new system implementation work requires careful planning and teamwork. Help from the government and new ways to pay for it can make AI in healthcare possible (Luong, 2024).
Data quality and availability challenges
Ensuring high-quality data is crucial for effective AI implementation in healthcare. However, several challenges exist:
- Inconsistent Data Formats Across Healthcare Systems: Different healthcare providers often use various data formats, making it difficult to integrate and analyze data efficiently (Krylov, 2024).
- Limited Access to Large, Diverse Datasets: AI systems require vast amounts of data to learn and make accurate predictions. However, accessing such datasets can be challenging due to privacy concerns and regulatory restrictions (Johns Hopkins Medicine, 2015).
- Ensuring Data Accuracy and Completeness: Inaccurate or incomplete data can lead to incorrect diagnoses and treatments, posing significant risks to patient safety (4medica, 2023).
Technical integration hurdles

Integrating AI into existing healthcare IT infrastructure presents several technical challenges:
- Compatibility Issues with Existing Healthcare IT Infrastructure: Many healthcare systems are built on legacy technologies that may not be compatible with modern AI solutions.
- Scalability Concerns for AI Systems: AI systems need to handle large volumes of data and scale efficiently as the amount of data grows.
- Maintenance and Updates of AI Algorithms: AI algorithms require regular updates to maintain accuracy and adapt to new medical knowledge.
How to address these technical challenges
Here are some ways to overcome these challenges:
- Developing Standardized Data Formats and APIs: Standardizing data formats and creating APIs can facilitate seamless data exchange between different systems (Krylov, 2024).
- Implementing Cloud-Based AI Solutions: Cloud-based solutions offer scalability and flexibility, making it easier to manage and update AI systems.
- Establishing Dedicated AI Support Teams: Having specialized teams to manage and support AI systems can ensure smooth integration and operation.
Following these guidelines will help when it comes to integrating an AI platform in a healthcare system.
Privacy and security concerns
Protecting patient data is paramount when implementing AI in healthcare. Some considerations include:
- Protecting Patient Data in AI Systems: AI systems must be designed with robust security measures to protect sensitive patient information (Yadav et al., 2023).
- Compliance with Healthcare Regulations: Ensuring compliance with regulations, like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S., is essential to avoid legal repercussions and maintain patient trust. The U.S. Food & Drug Administration (FDA) focuses on approving AI developers. Europe has made laws and data protection rules for AI use (Murdoch, 2021).
- Managing Consent for AI Use in Patient Care: Obtaining and managing patient consent for using their data in AI systems is crucial for ethical and legal compliance.
AI and HIPAA Compliance

Balancing data use for AI with patient privacy rights is a key issue.
AI needs lots of data, more than clinical trials usually have. Some areas like eye care do well with this. However, sharing data can risk patient privacy, affecting jobs, insurance, or identity theft. It’s hard to hide patient info completely (Alonso & Siracuse, 2023).
For rare diseases, data from many places is needed. Sharing data can increase privacy risks, like identifying patients from anonymous data. Working with big companies raises concerns about data being used for profit, which can clash with fair data use (Tom et al., 2020).
AI tools that learn over time might accidentally break HIPAA rules. Doctors must understand how AI handles patient data to follow HIPAA rules. They need to know where AI gets its info and how it’s protected. Healthcare workers must use AI responsibly, get patient permission, and be open about using AI in care (Accountable HQ, 2023).
AI in healthcare needs rules that respect patient rights. We should focus on letting patients choose how their info is used. This means asking for permission often, and making it easy for patients to take back their data if they want to.
We also need better ways to protect patient privacy. Companies holding patient data should use the best safety methods and follow standards. If laws and standards don’t keep up with fast-changing tech like AI, we’ll fall behind in protecting patients’ rights and data (Murdoch, 2021).
Copyright issues
When using AI in clinical research, copyright problems can occur because AI uses information from many places to make content. It might use copyrighted content without knowing, causing legal issues. It’s important to make sure AI doesn’t use protected material (Das, 2024).
Ethical and legal concerns

We need strong laws and data standards to manage AI use, especially in the field of medicine. Ethical and legal issues are significant barriers to using AI in healthcare, for example:
- Addressing Bias in AI Algorithms: AI systems can inherit biases present in training data, leading to unequal treatment outcomes.
- Establishing Liability in AI-Assisted Decisions: AI and the Internet of Things (IoT) technologies make it hard to decide who’s responsible when things go wrong (Eldadak et al., 2024). We need clear guidelines on who is liable for errors made by AI systems–AI developers, the doctor, or the AI itself (Cestonaro et al., 2023).
- Creating Transparency in AI Decision-Making Processes: AI systems should be transparent in their decision-making processes to build trust among clinicians and patients.
How to address these ethical concerns
We should think about how these technologies affect patients and what risks they should take. We need to find a balance that protects people without stopping new ideas. Ways to overcome some of these barriers include:
- Developing AI Ethics Committees in Healthcare Institutions: Ethics committees can oversee AI implementations and ensure they adhere to ethical standards.
- Creating Clear Guidelines for AI Use in Clinical Settings: Establishing guidelines can help standardize AI use and address ethical and legal concerns.
- Engaging in Ongoing Dialogue with Legal and Ethical Experts: Continuous engagement with experts can help navigate the evolving ethical and legal landscape.
Scientists, colleges, healthcare organizations, and regulatory agencies should work together to create standards for naming data, sharing data, and explaining how AI works. They should also make sure AI code and tools are easy to use and share (Wang et al., 2020).
The old ways of dealing with legal problems don’t work well for AI issues. We need a new approach that involves doctors, AI makers, insurance companies, and lawyers working together (Eldadak, et al., 2024).
Resistance to change and adoption

Resistance from healthcare professionals can hinder AI adoption for many reasons:
- Overcoming Clinician Skepticism Towards AI: Educating clinicians about the benefits and limitations of AI can help reduce skepticism.
- Addressing Fears of AI Replacing Human Roles: Emphasizing AI as a tool to add to, not replace, human roles can alleviate fears.
- Managing the Learning Curve for New AI Tools: Providing adequate training and support can help clinicians adapt to new AI tools.
AI might not work well with new data in hospitals, which could harm patients. There are many issues with using AI in medicine. These include lack of proof it’s better than old methods, and concerns about who’s at fault for mistakes (Guarda, 2019).
Training and education gaps

Lack of AI literacy among healthcare professionals is a significant barrier:
- Lack of AI Literacy Among Healthcare Professionals: Many clinicians lack the knowledge and skills to effectively use AI tools.
- Limited AI-Focused Curricula in Medical Education: Medical schools often do not include comprehensive AI training in their curricula.
- Keeping Pace with Rapidly Evolving AI Technologies: Continuous education is necessary to keep up with the fast-paced advancements in AI.
How to address these knowledge gaps
We can bridge the knowledge gap by:
- Integrating AI Training into Medical School Curricula: Incorporating AI education into medical training can prepare future clinicians for AI integration.
- Offering Continuous Education Programs for Practicing Clinicians: Regular training programs can help practicing clinicians stay updated on AI advancements.
- Developing User-Friendly AI Interfaces for Clinical Use: Designing intuitive AI tools can make it easier for clinicians to adopt and use them effectively.
Doctor-patient knowledge sharing

Healthcare providers need to understand AI to explain it to patients. They don’t need to be experts, but according to Cascella (n.d.), they should know enough to:
- Explain how AI works in simple terms.
- Share their experience using AI.
- Compare AI’s risks and benefits to human care.
- Describe how humans and AI work together.
- Explain safety measures, like double-checking AI results.
- Discuss how patient information is kept private.
Doctors should take time to explain these things to patients and answer questions. This helps patients make good choices about their care. After talking, doctors should write down what they discussed in the patient’s records and keep any permission forms.
By doing this, doctors make sure patients understand and agree to AI use in their care. Patients should understand how AI might affect their treatment and privacy.
How to Implement AI Platforms in Healthcare

Here are the technical steps that Tateeda (2024) recommends to implement the technical aspects of AI into an existing healthcare system:
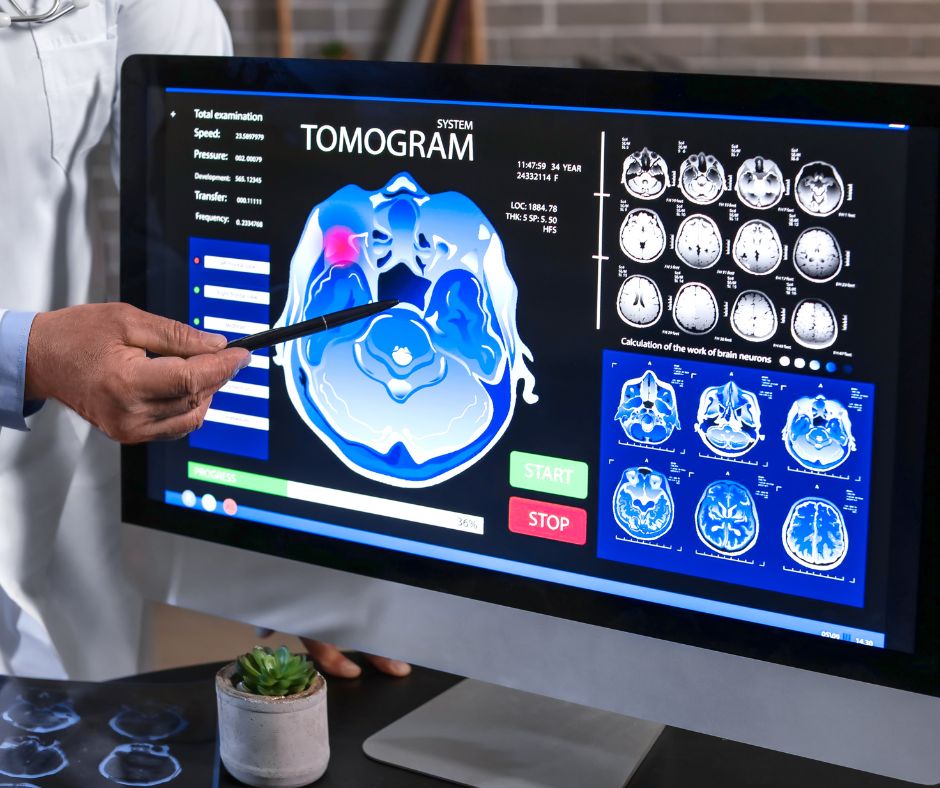
- Prepare the data: Collect health info like patient records and medical images. Clean it up, remove names, and store it safely following data privacy standards.
- Choose your AI model: Choose where AI can help, like disease diagnosis or patient monitoring. Select AI that fits these jobs, like special programs for looking at images or predicting health risks.
- Train the AI model: Teach the AI using lots of quality health data. Work with doctors to make sure the AI learns the right things.
- Set up and test the model: Integrate AI into the current health system(s). Check it works well by testing it a lot and asking doctors what they think.
- Use and monitor: Start using AI in hospitals. Make sure it works within the processes doctors are accustomed to. Keep an eye on how it’s doing and get feedback to continue making it better.
Conclusion
To implement AI in clinical practice with success, we must address data quality, technical integration, privacy, ethics, and education, challenges. Healthcare providers can pave the way for successful AI adoption in clinical practice–the key lies in a multifaceted approach to:
- Invest in robust IT infrastructure
- Foster a culture of continuous learning
- Maintain open dialogue among all stakeholders.
As we navigate these hurdles, the healthcare industry moves closer to a future where AI seamlessly enhances clinical practice, ultimately leading to better outcomes for patients and more efficient systems for providers.
References
AI in Healthcare: What it means for HIPAA. (2023). Accountable HQ. Retrieved from https://www.accountablehq.com/post/ai-and-hipaa
Alonso, A., Siracuse, J. J. (2023). Protecting patient safety and privacy in the era of artificial intelligence. Seminars in Vascular Surgery 36(3):426–9. https://pubmed.ncbi.nlm.nih.gov/37863615/
American Medical Association (AMA). (2023). Physician sentiments around the use of AI in health care: motivations, opportunities, risks, and use cases. AMA Augmented Intelligence Research. Retrieved from https://www.ama-assn.org/system/files/physician-ai-sentiment-report.pdf
Cascella, L. M. (n.d.). Artificial Intelligence and Informed Consent. MedPro Group. Retrieved from https://www.medpro.com/artificial-intelligence-informedconsent
Cestonaro, C., Delicati, A., Marcante, B., Caenazzo, L., & Tozzo, P. (2023). Defining medical liability when artificial intelligence is applied on diagnostic algorithms: A systematic review. Frontiers in Medicine, 10. doi.org/10.3389/fmed.2023.1305756
Das, S. (2024). Embracing the Future: Opportunities and Challenges of AI integration in Healthcare. The Association of Clinical Research Professionals (ACRP). Clinical Researcher, 38(1). Retrieved from https://acrpnet.org/2024/02/16/embracing-the-future-opportunities-and-challenges-of-ai-integration-in-healthcare
Data Quality Issues in Healthcare: Understanding the Importance and Solutions. (2024). 4Medica. Retrieved from https://www.4medica.com/data-quality-issues-in-healthcare/
Definition of Limited Data Set. (2015). Johns Hopkins Medicine. Retrieved from https://www.hopkinsmedicine.org/institutional-review-board/hipaa-research/limited-data-set
Eldakak, A., Alremeithi, A., Dahiyat, E., Mohamed, H., & Abdulrahim Abdulla, M. I. (2024). Civil liability for the actions of autonomous AI in healthcare: An invitation to further contemplation. Humanities and Social Sciences Communications, 11(1), 1-8. doi.org/10.1057/s41599-024-02806-y
Guarda, P. (2019.) ‘Ok Google, am I sick?’: artificial intelligence, e-health, and data protection regulation. BioLaw Journal (Rivista di BioDiritto) (1):359–75. https://teseo.unitn.it/biolaw/article/view/1336
Krylov, A. (2024). The Value and Importance of Data Quality in Healthcare. Kodjin. Retrieved from https://www.kodjin.com/blog/the-value-and-importance-of-data-quality-in-healthcare
Luong, K. (2024). Challenges of AI Integration in Healthcare. Ominext. Retrieved from https://www.ominext.com/en/blog/challenges-of-ai-integration-in-healthcare
Mittermaier, M., Raza, M. M., & Kvedar, J. C. (2023). Bias in AI-based models for medical applications: challenges and mitigation strategies. Npj Digital Medicine, 6(113). doi.org/10.1038/s41746-023-00858-z
Murdoch, B. (2021). Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Med Ethics 22(1):1–5.
Top 5 Use Case of AI in Healthcare: Implementation Strategies and Future Trends. (2024). Tateeda. Retrieved from https://tateeda.com/blog/ai-in-healthcare-use-cases
Tom, E., Keane, P. A., Blazes, M., Pasquale, L. R., Chiang, M. F., Lee, A. Y., et al. (2020). Protecting Data Privacy in the Age of AI-Enabled Ophthalmology. Transl Vis Sci Technol 9(2):36–6. doi.org/10.1167/tvst.9.2.36
Wang, S. Y., Pershing, S., & Lee, A. Y. (2020). Big Data Requirements for Artificial Intelligence. Current Opinion in Ophthalmology, 31(5), 318. doi.org/10.1097/ICU.0000000000000676
Yadav, N., Pandey, S., Gupta, A., Dudani, P., Gupta, S., & Rangarajan, K. (2023). Data Privacy in Healthcare: In the Era of Artificial Intelligence. Indian Dermatology Online Journal, 14(6), 788-792. doi.org/10.4103/idoj.idoj_543_23