As our population ages, ensuring the safety and well-being of seniors living independently has never been greater. A study by AARP shows that 77% of older adults want to age in place, making remote monitoring technologies more relevant than ever. Remote monitoring for seniors is a powerful tool that can help older adults age in place safely, and give their families and caregivers peace of mind.
In this article, we’ll discuss the benefits and available technologies for remote monitoring for seniors, and how to implement these systems effectively.
Contents
Understanding Remote Monitoring for Seniors
Remote monitoring for seniors refers to the use of technology to track an older adult’s health, safety, and well-being from a distance. These systems allow caregivers and healthcare providers to keep an eye on seniors without being physically present, enabling quick responses to emergencies and early detection of potential health issues.

What are the types of remote monitoring systems?
There are several types of remote monitoring systems available for seniors:
- Wearable devices
- Smart home sensors
- Video monitoring systems
- Health tracking devices
- Personal emergency response systems (PERS)
Each type of system serves different purposes and can be tailored to meet the specific needs of individual seniors.
Key components of an effective remote monitoring setup
An effective remote monitoring setup typically includes:
- Sensors or devices to collect data
- A central hub or gateway to process and transmit information
- A user interface for caregivers to access and interpret data
- Alert systems for emergencies or anomalies
- Secure data storage and transmission protocols
These components work together to create a comprehensive monitoring solution that can adapt to various care scenarios.
Benefits of Remote Senior Monitoring
Remote monitoring offers numerous advantages for both seniors and their caregivers. Let’s examine some of the key benefits.
Enhanced safety and quick emergency response

One of the primary benefits of remote monitoring is improved safety for seniors. These systems can detect falls, unusual inactivity, or other emergencies and automatically alert caregivers or emergency services.
Researchers in the UAE and the U.K. ran a study where they created a system to detect falls, and to monitor seniors and people with disabilities. The non-intrusive system uses Wi-Fi signals and AI to analyze movement patterns without cameras or wearable devices. Overall, this technology offers a promising way to improve safety and care for vulnerable populations using everyday Wi-Fi signals and smart AI analysis (Al Rajab et al., 2023).
Increased independence for seniors
Remote monitoring allows seniors to maintain their independence while still receiving necessary support. By providing a safety net, these systems give older adults the confidence to continue living in their own homes.
Reduced caregiver stress

For family caregivers, remote monitoring, including mobile health apps, can significantly reduce stress and anxiety (Fuller-Tyszkiewicz et al., 2020). Knowing that they can check on their loved one’s well-being at any time provides invaluable peace of mind
Cost-effectiveness compared to in-person care
Remote monitoring can be a cost-effective alternative to full-time in-person care or assisted living facilities. While initial setup costs may be significant, the long-term savings can be substantial.
According to a report by Grand View Research, the global remote patient monitoring market is expected to reach $117.1 billion by 2025, driven in part by its cost-effectiveness. It’s expected to register a compound annual growth rate (CAGR) of 18.6% from 2024 to 2030.
Top Remote Monitoring Technologies for Seniors
Let’s explore some of the most popular and effective remote monitoring technologies available for seniors.
Wearable devices and personal emergency response systems (PERS)

Wearable devices, such as smartwatches or pendants, can track vital signs, detect falls, and allow seniors to call for help with the push of a button. These devices are often waterproof and can be worn 24/7 for continuous protection.
Example: The Apple Watch Series includes fall detection and an ECG app, making it a popular choice for tech-savvy seniors.
Smart home sensors and environmental monitoring

Smart home sensors can be placed throughout a senior’s living space to monitor movement, temperature, and other environmental factors. These sensors can detect unusual patterns that may indicate a problem.
Example: Caregiver Smart Solutions offers a system of small sensors that can be placed around the home to track daily habits and alert caregivers to changes in routine.
Video monitoring and two-way communication systems
Video monitoring systems allow caregivers to visually check in on seniors and communicate with them face-to-face. These systems are especially important for seniors with mobility issues or those who live far from family members.
Example: The GrandCare Systems platform includes video chat capabilities along with other monitoring features.
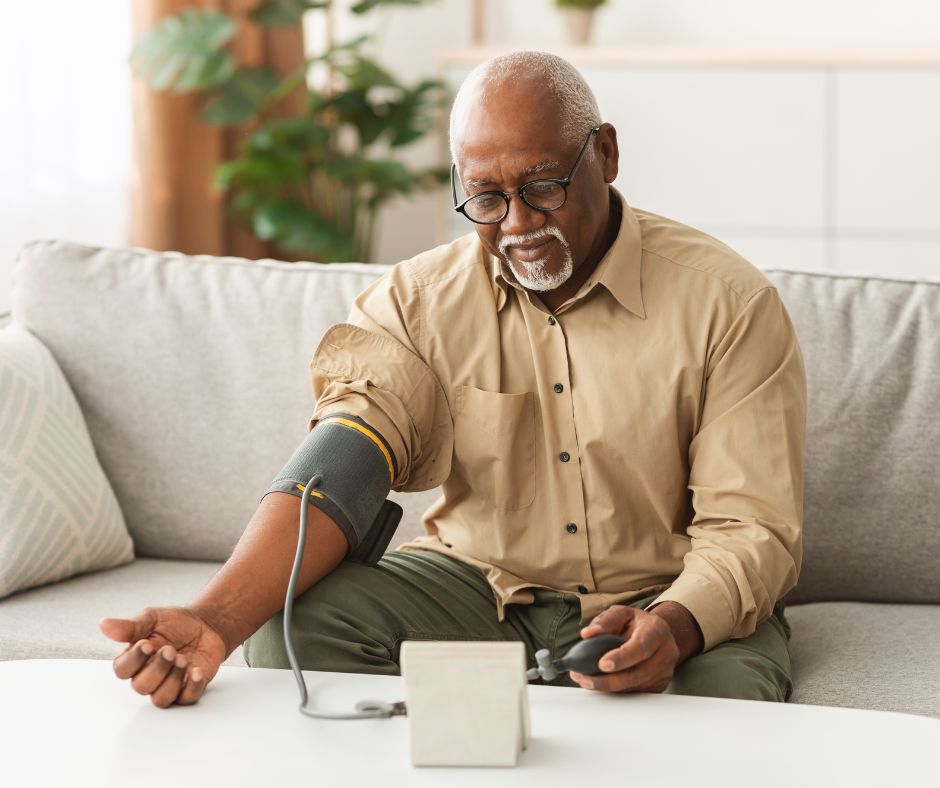
Health tracking devices and telemedicine integration
Health tracking devices can monitor vital signs, medication adherence, and other health metrics. Many of these devices integrate with telemedicine platforms, allowing healthcare providers to remotely assess a senior’s condition.
Example: The Livongo (by Teladoc Health) remote monitoring system includes a blood glucose meter and blood pressure monitor that automatically shares data with healthcare providers.
Health tracking for seniors in nursing homes

A study published in Fusion introduced a new way to predict personal health for older people in nursing care using a model to estimate health conditions without needing special sensors. The method looks at actions in each area and combines information from different sources to make better predictions. It also uses machine learning and other smart techniques to process and combine data.
This model works better than existing systems for tracking health without extra sensors. It could be used with wearable devices in the future to improve health monitoring for seniors (Mahmood et al., 2023).
Implementing Remote Monitoring: A Step-by-Step Guide
If you’re considering implementing a remote monitoring system for a senior loved one, follow these steps:
- Assess individual needs and preferences.
- Choose the right technology for your situation.
- Set up the system and ensure proper connectivity.
- Train seniors and caregivers on system use.
Assess individual needs and preferences

Start by evaluating the senior’s specific health concerns, living situation, and personal preferences. Consider factors such as:
- Mobility level
- Cognitive function
- Existing health conditions
- Technology comfort level
- Privacy concerns
Choose the right technology for your situation
Based on your assessment, research and select the most appropriate monitoring technology. Consider factors like:
- Ease of use
- Cost and ongoing fees
- Integration with existing devices or systems
- Customer support and reliability
Set up the system and check for proper connectivity

Once you’ve chosen a system, follow these steps for setup:
- Install any necessary hardware or sensors.
- Set up the central hub or gateway.
- Test connectivity and ensure all components are communicating properly.
- Configure alert settings and user preferences.
Train seniors and caregivers
Proper training is crucial for the success of any remote monitoring system. Be sure to:
- Provide clear, step-by-step instructions for both seniors and caregivers.
- Offer hands-on practice with the devices or interface.
- Address any concerns or questions about the system.
- Schedule follow-up training sessions as needed.
Addressing Privacy and Ethical Concerns
While remote monitoring offers many benefits, it’s essential to address privacy and ethical concerns.

Balance safety with personal privacy
Striking the right balance between safety and privacy is crucial. Consider these tips:
- Involve the senior in decisions about monitoring.
- Use the least invasive monitoring methods that meet safety needs.
- Establish clear boundaries for when and how monitoring will be used.
Ensure data security and protection
Protecting sensitive health data is paramount. Look for systems that offer:
- End-to-end encryption
- Secure cloud storage
- Regular security updates
- Compliance with healthcare privacy regulations (like HIPAA)
Get consent and involve seniors in decision-making
Always obtain informed consent from the senior before implementing any monitoring system:
- Explain the purpose and functionality of the system
- Discuss potential benefits and risks
- Address any concerns or questions
- Respect the senior’s right to refuse or limit monitoring
Future Trends in Remote Senior Monitoring
The field of remote senior monitoring is rapidly evolving.
AI and predictive analytics
AI-powered systems can analyze data from multiple sources to predict potential health issues before they become serious. For example, researchers at the University of Missouri developed a system that uses AI to detect early signs of illness in seniors based on changes in their daily routines.
Integration with smart home ecosystems

As smart home technology becomes more prevalent, remote monitoring systems are getting easier to integrate with these ecosystems. This allows more comprehensive monitoring and easier control of the home environment.
Advancements in non-invasive health monitoring
New technologies allow us to monitor health metrics without the need for wearable devices or invasive procedures. For instance, researchers at MIT developed a wireless device that can monitor sleep patterns and detect abnormalities without any physical contact.
Conclusion
Remote monitoring for seniors is a rapidly growing field that offers significant benefits for both older adults and their caregivers. By enhancing safety, promoting independence, and providing peace of mind, these technologies are helping seniors age in place with dignity and confidence.
Before you choose a remote monitoring system, remember to carefully assess individual needs, involve your senior family members in the decision-making process, choose appropriate technology, and address privacy concerns.
With the right approach, remote monitoring can be a valuable tool to support our elderly loved ones with the care they need while respecting their autonomy.
References
Al-Rajab, M., Al Zraiqat, S., John, K., El Ayoubi, M. B., & Qassem, M. O. (2023). A Contactless Smart WiFi-Based Application Presence or Fall Detection System: Analyzing Channel State Information (CSI) Signals. International Journal of Emerging Multidisciplinaries: Computer Science & Artificial Intelligence; 2(1). doi.org/10.54938/ijemdcsai.2023.02.1.230
Binette, J. & Fanni, F. (2021). 2021 Home and Community Preference Survey: A National Survey of Adults Age 18-Plus. Washington, DC: AARP Research. doi.org/10.26419/res.00479.001
Diabetes made easier at no cost to you. (n.d.). Livongo. Retrieved from https://www.livongo.com/diabetes
Fuller-Tyszkiewicz, M., Richardson, B., Little, K., Teague, S., Hartley-Clark, L., Capic, T., Khor, S., Cummins, R. A., Olsson, C. A., & Hutchinson, D. (2020). Efficacy of a Smartphone App Intervention for Reducing Caregiver Stress: Randomized Controlled Trial. Journal of Medical Internet Research Mental Health; 7(7). doi.org/10.2196/17541
Grand View Research. (2024). Remote Patient Monitoring Market Size, Share & Trends Analysis Report By Product (Vital Sign Monitor, Specialized Monitor), By End-use (Hospital Based Patient, Ambulatory Patient), By Application, By Region, And Segment Forecasts, 2024 – 2030. Retrieved from https://www.grandviewresearch.com/industry-analysis/remote-patient-monitoring-devices-market
Ham, B. (2020). Wireless device captures sleep data without using cameras or body sensors. MIT News. Retrieved from https://news.mit.edu/2020/monitoring-sleep-sensors-0911
Herd, R. (2024). Technology Tips for Caregivers: How to Use Monitoring Systems for Peace of Mind. Caregiver Smart Solutions. Retrieved from https://www.caregiversmartsolutions.com/post/technology-tips-for-caregivers-how-to-use-monitoring-systems-for-peace-of-mind
How GrandCare Works. (n.d.). GrandCare Systems. Retrieved from https://www.grandcare.com/how-it-works/
Ianzito, C. (2020). Remote Monitoring Systems Can Give Caregivers Peace of Mind. AARP. Retrieved from https://www.aarp.org/caregiving/home-care/info-2020/ces-caregiving-products.html
Mahmood, H., Faleh, H., Khalid, R., & Al-Kikani, S. (2023). Physical Activity Monitoring for Older Adults through IoT and Wearable Devices: Leveraging Data Fusion Techniques. Fusion: Practice and Applications; 11(2), pp. 48-61. doi.org/10.54216/FPA.110204
Rice, S. (2016). Sensor Systems Identify Senior Citizens at Risk of Falling Within Three Weeks. University of Missouri. Retrieved from https://www.eldertech.missouri.edu/sensor-systems-identify-senior-citizens-at-risk-of-falling-within-three-weeks/